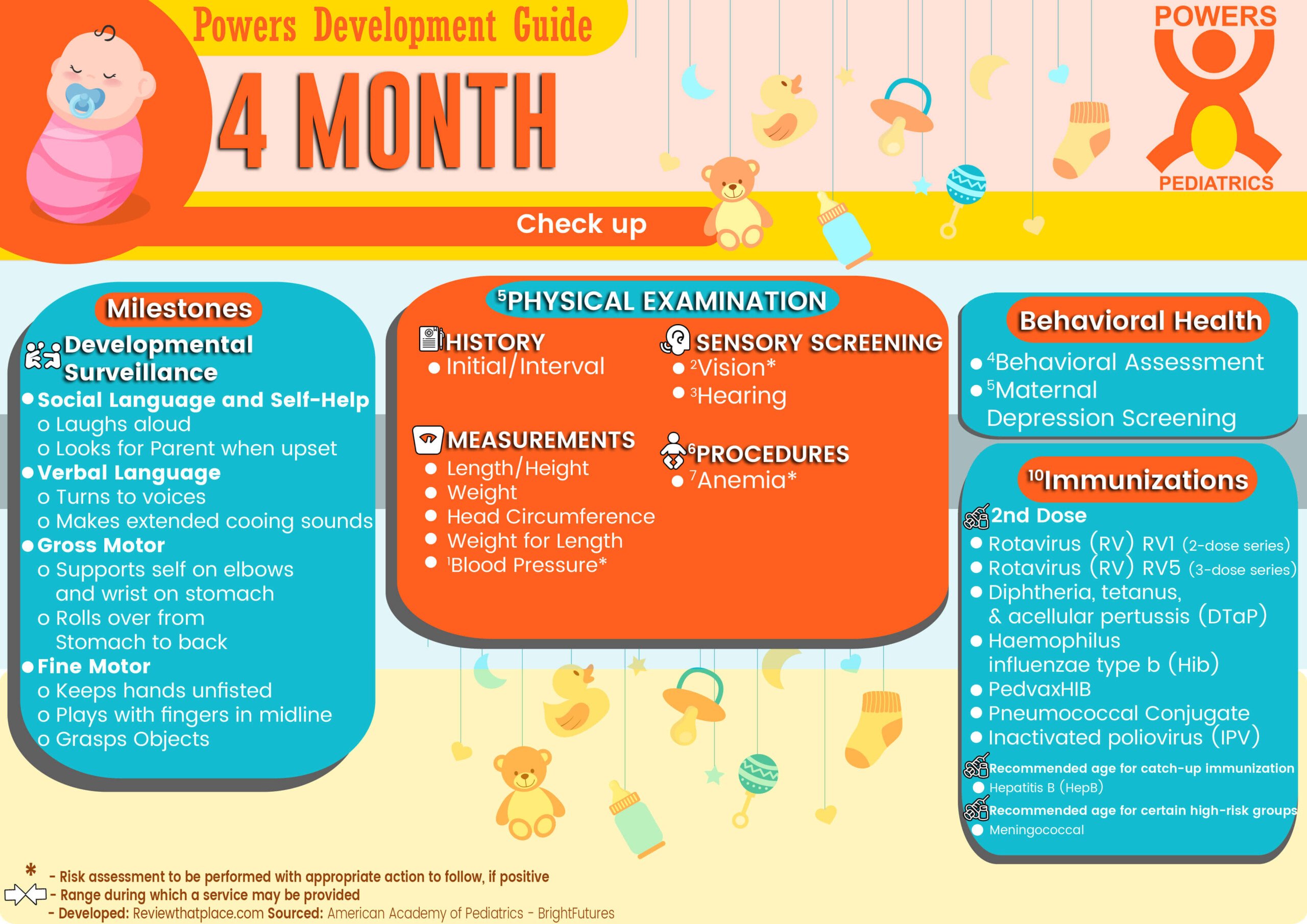
What to expect during a 4-Month-Old Physical
Developmental Surveillance
- Social Language and Self-Help
- Laughs aloud
- Looks for Parent when upset
- Verbal Language
- Turns to voices
- Makes extended cooing sounds
- Gross Motor
- Supports self on elbows and wrist on stomach
- Rolls over from Stomach to back
- Fine Motor
- Keeps hands unfisted
- Plays with fingers in the midline
- Grasps Objects
BEHAVIORAL HEALTH
3PHYSICAL EXAMINATION
- HISTORY
- Initial/Interval
- MEASUREMENTS
- Length/Height and Weight
- Head Circumference
- Weight for Length
- 4 Blood Pressure*
- SENSORY SCREENING
- 5 Vision*
- Hearing*
- PROCEDURES
- These may be modified, depending on entry point into schedule and individual need.
6 Immunization
- Recommended age for catch-up immunization
- Hepatitis B (HepB)
- Recommended age for certain high-risk groups
- Meningococcal (MenACWY-D ≥9 mos; MenACWY-CRM ≥2 mos)
- 2nd Dose Rotavirus (RV) RV1 (2-dose series)
- 2nd Dose Rotavirus (RV) RV5 (3-dose series)
- 2nd Dose Diphtheria, tetanus, & acellular pertussis (DTaP:<7 yrs)
- 2nd Dose Haemophilus influenza type b (Hib)
- 2nd Dose PedvaxHIB
- 2nd Dose Pneumococcal conjugate (PCV13)
- 2nd Dose Inactivated poliovirus (IPV: <18 yrs)
- 7 Anemia*
* risk assessment to be performed with appropriate action to follow, if positive
4-Month-Old Anticipatory Guidance
Social Determinants of Health
◊ Risks (environmental risk: lead, work-related exposures) ◊ Strengths and Protective Factors (family relationships and support, child care)
- Reduce lead exposure at home
- Maintain social contacts
- Make time for self, partner
- Spend time with your other children.
- Make quality childcare arrangements.
Infant behavior and development
◊ Infant Self-Calming
◊ Parent-Infant Communication
◊ Consistent Daily Routines ◊ Media ◊ Playtime
- What do you do to calm your baby? What do you do if that does not work? Do you ever feel that you and/or other caregivers may hurt the baby?
- Continue calming strategies when the baby is fussy.
- Spend time talking/playing with the baby.
- Create a daily routine for feeding /naps/bedtime.
- Avoid TV and other digital media with the baby.
- Use quiet (reading, singing) and active (“tummy time”) playtime
- provide safe opportunities to explore.
Oral Health
◊ Maternal Oral Health ◊ Teething and Drooling ◊ Good Oral Hygiene (no bottle in bed)
- Don’t share spoons; don’t clean pacifiers in your mouth; maintain good dental hygiene.
- Use a cold teething ring to relieve teething pain.
- Don’t put the baby in a crib with a bottle; never prop a bottle when feeding.
- Clean teeth /gums 2 times per day; use a soft cloth/toothbrush with tap water and a small smear of fluoridated toothpaste (no more than a grain of rice).
Nutrition and feeding
◊ General Guidance on Feeding
◊ Feeding Choices (avoid grazing)
◊ Delaying Solid Foods
◊ Breastfeeding Guidance
◊ Supplements and Over-The-Counter Medications
◊ Formula Feeding Guidance
- Exclusive breastfeeding for about the first 6 months is ideal
- The iron-fortified formula is recommended substitute.
- Delay solid foods until baby is 6 months old.
- If breastfeeding:
- Recognize growth spurts
- Give baby vitamin D (400 IU per day)
- Begin infant iron supplementation
- Discuss safe pumping/ storing breast milk
- Report any medications/ supplements /herbs /vitamins.
- If formula feeding:
- Prepare /store formula safely
- 8 to 12 times in 24 hours; 30 to 32 oz total
- hold baby semi-up right
- consider contacting WIC.
Safety
◊ Car Safety Seats ◊ Safe Asleep ◊ Safe Home Environment
- Car Seats
- Use a rear-facing car safety seat in the backseat
- Never put the baby in the front seat of a vehicle with a passenger airbag
- Keep the baby in a car safety seat at all times during travel.
- Use a seat belt; don’t drive after using alcohol or drugs.
- Put baby to sleep on back; choose the crib with slats less than 2¾” apart; don’t use loose, soft bedding;
- Avoid burn risk while holding a baby (drinking hot liquids, cooking, ironing, smoking)
- Set the home water temperature to less than 120°F.
- Don’t leave baby alone in:
- Tub
- High places (changing tables, beds, sofas)
- Keep a hand on the baby (“touch supervision”).
- Keep small objects, and plastic bags away from the baby. Avoid infant walkers.
Goals For 4-Month Checkup:
- Be gentle and patient
- Get more sleep
- Make a budget
- Leave your work at the office
- Focus on self-care
- Meditate as a family
- Find an outlet
- “cell-free” zone
- Spend more time with your partner
- Take more baths
- Have a girls’/boys’ night
- Be more flexible
- See your child for who they are
- Teach your child to speak up
- Help those less fortunate
- Drink more water
- Find 30 minutes a day of “me” time
- Challenge yourself
- Focus on experiences, not things
- Make health a priority
- Start—or finish—a degree
- Inform yourself
- Maintain balance
- Laugh often
- Cook dinner more frequently
- Ask for help
- Have designated “cheat” days
- Stop having FOMO
- Say “I love you” more often.
- This assessment should be family-centered and may include an assessment of the child’s social-emotional health, caregiver depression, and social determinants of health. [Reference] ↩︎
- Screening should occur per. [Reference] ↩︎
- At each visit, age-appropriate physical examination is essential, with infants totally unclothed and older children undressed and suitably draped. The extent of the physical examination is determined by both the reason for the visit and diagnostic considerations raised during the taking of the history. [Reference] ↩︎
- Blood pressure measurement in infants and children with specific risk conditions should be performed at visits before age 3 years. [Reference] ↩︎
- Instrument-based screening may be used to assess risk at ages 12 and 24 months. [Reference] ↩︎
- Every visit should be an opportunity to update and complete a child’s immunizations.[Reference] ↩︎
- Perform risk assessment or screening, as appropriate, per recommendations in the current edition of the AAP Pediatric Nutrition. ↩︎